COVID-19: Interim Guidance
Update: The COVID-19 national emergency and public health emergency (PHE) ended on May 11, 2023. As a result, Evernorth’s cost-share waiver for diagnostic COVID-19 tests and related office visits ends on May 12, 2023.
Individual providers and outpatient clinics may permanently use telehealth for outpatient therapy, applied behavior analysis (ABA)*, medication management, and Employee Assistance Program (EAP) services. The expiration of the PHE does not apply to these telehealth services.
* Medical Necessity Criteria for the level of care being delivered must continue to be met.
Coverage of behavioral telehealth sessions
Behavioral telehealth sessions are available to covered patients and are administered in accordance with their behavioral health benefits. Prior to rendering services, you should verify behavioral health benefits and eligibility for all plan types, including services administered by a third-party administrator, by calling the number on the back of the patient’s ID card. An "S" identifier on the bottom left of the card can help you identify which of your patients have services administered by a third-party administrator.
Individual providers and outpatient clinics
If you are an individual provider or an outpatient clinic, you may permanently use telehealth for outpatient therapy, applied behavior analysis (ABA),* medication management, and Employee Assistance Program (EAP) services. The expiration of the PHE does not apply to the telehealth services noted above.
You may offer telephonic sessions to patients who do not have access to technology to participate in telehealth sessions, as appropriate and in accordance with current legislative guidance. Include the following information on your claim form:
- Appropriate Current Procedural Terminology® (CPT®) code in Field 24-D for the service(s) provided
- Modifier 95** in Field 24-D to specify telehealth (see sample claim below)
- Place of Service (POS) 02 in Field 24-B (see sample claim form below)
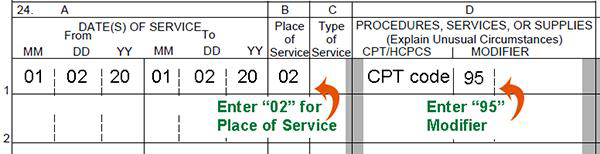
For illustrative purposes only.
Facilities
Facilities can render some or all of their services via telehealth (i.e., PHP, IOP, or services that are offered within an inpatient stay such as attending consultations or family therapy sessions), if appropriate. Providers may offer telephonic sessions to patients who do not have access to technology to participate in telehealth sessions, as appropriate and in accordance with current legislative guidance.
- If a facility normally bills services on a UB04 claim form, they must include the following on their claim:
- Appropriate Revenue Code for the service rendered
- Appropriate CPT® or Healthcare Common Procedure Coding System (HCPCS) code for the service rendered
- Modifier 95**
- If routine outpatient services are normally billed on a CMS1500 claim form, the following must be included:
- Modifier 95** in Field 24-D to specify telehealth (see sample claim above)
- 02 in Place of Service in Field 24-B (see sample claim above)
* Medical Necessity Criteria for the level of care being delivered must continue to be met.
** The "GT" modifier has been retired by the Centers for Medicare & Medicaid Services (CMS), but it still acceptable on claim forms.
Additional resources
- If you have additional questions about providing behavioral telehealth sessions to covered patients, call Provider Services at 800.926.2273.
Resources to support
your mental health
Live-guided relaxation by telephone
- Available for all providers at no cost
- Every Tuesday at 5:00pm ET
- Call 866.205.5379, enter passcode 113 29 178, and then press #